Background: By day, I write and teach my students on CaseInterview.com about how to have a successful career. By night, I volunteer with my county as an emergency worker, search & rescue team member, and emergency medical responder. Much of my training is in mass casualty incidents.
Under normal circumstances, medical care in the United States is based on the principle of “do what’s best for the patient.” However, this rule changes quite profoundly during a situation known as a Mass Casualty Incident (MCI). During an MCI, the guideline changes to “do the most good for the most people.” This has major implications for who gets a hospital bed during the current coronavirus epidemic.
Let me explain.
An MCI is defined as any situation when the # of patients exceeds your capacity to care for them. This could result from a shortage of personnel, equipment, medications, or access to transportation to higher levels of care (e.g., ambulances).
During an MCI, we intentionally do not treat extremely severe patients that are unlikely to live. For example, in regular situations, if a patient stops breathing in the field, we would do CPR. During an MCI (such as an earthquake), if they are not breathing, we tilt their chin back to open their airway. If they start breathing on their own, that’s great. If they don’t, we tag them with a black tag indicating the patient is dead or “expectant” (expected to die) and walk away.
The reason we do this is that multi-hour CPR in the field requires 15-20 people. (CPR requires 90 chest compressions every minute. So, imagine doing 90 quasi-push-ups per minute for 5 hours until help can arrive. In those 300 minutes, that’s 27,000 “push-ups.” One person likely cannot do that alone and will need others to swap in during that time.)
In an earthquake (the MCI scenario we train for most), it might take many hours to get a patient to a hospital and doing CPR for that length of time is extremely resource-intensive. The thinking is that those 15 or so first responders who are all working on one patient could instead be treating many other patients’ survivable bleeding injuries, splinting broken bones, etc…
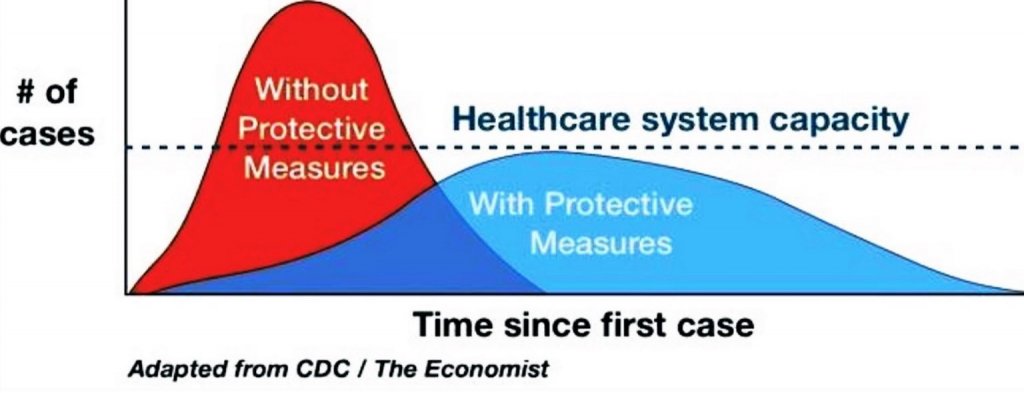
Now, let’s get to the coronavirus and hospital beds. With new infections currently on an exponential growth curve, there’s a very serious risk of the # of patients requiring hospitalization exceeding the # of available hospital beds. On March 10, 2020, the entire country of Italy was put on lockdown. One of THE primary reasons for this is that the hospitals in certain regions have already been overwhelmed. In short, there are more patients needing hospital beds than beds available.
What Italian medical professionals have been struggling with, psychologically, are the new triage rules in place. In Italy, extremely ill, elderly patients with high-risk factors do not get hospital beds. Italian nurses and doctors have been instructed to give hospital beds to younger patients that would almost certainly survive if given proper treatment. In other words, they are intentionally letting some patients die.
When I trained to make these decisions in the field, I had a really hard time with it. Could I really walk away from a patient that was still living (barely) and just let them die? If I didn’t walk away, was I really willing to risk the lives of the 5-10 other patients I could otherwise treat? If I didn’t walk away, would I really ask 10 of my colleagues to help, and risk the lives of 50-100 patients?
By pure math and logic, the answer is simple. Sacrifice the one to save the 50-100. Emotionally and psychologically, that’s a sobering and dark thought.
The reality is that MCI rules focus on a simple guideline — “do the most good, for the most people.” At the end of the coronavirus epidemic, you want the most people possible to survive. In a resource-constrained environment, that necessitates not treating a patient that consumes too many resources or is not likely to survive even with treatment. Once the number of patients exceeds hospital resources, everything changes. Some very difficult decisions will be made regarding who lives and who dies.
This is why the goal in the United States has shifted from containing the virus to slowing it down sufficiently. The goal is to do everything possible to make sure we don’t run out of hospital beds. Some deaths from the coronavirus will be unavoidable. However, dying because the hospital ran out of beds is, in many cases, a preventable death.
For more on this concept, visit www.FlattenTheCurve.com
